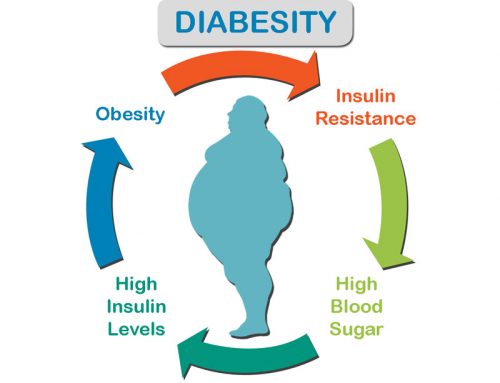
Chronic low-grade inflammation seems to play a role in all of the major diseases — heart disease, diabetes, arthritis, and certain cancers. Chronic inflammation fuels many of the devastating complications of type 2 diabetes, including cardiovascular, kidney, periodontal diseases and even cancers. The association between inflammation and diabetes is well-known and hyperglycemia itself is a proinflammatory condition leading to an increase in inflammatory markers in blood. Inflammation has a key role in the pathophysiology of type 2 diabetes and its associated metabolic abnormalities. Hyperglycemia leads to oxidative stress, which further results in inflammation. Insulin Resistance, commonly as a manifestation of hyperglycemia, is pro-inflammatory. So, does lowering blood sugars lower inflammation?
For years, it was assumed that that tight blood glucose control would reduce the complications of Type 2 Diabetes. After all, most diabetics die of cardio vascular disease and therefore, any strategy that reduced cardiovascular disease would be important. So, around 2008, four major trials (ACCORD, ADVANCE, VADT, and ORIGIN) were published to the question of whether lowering blood sugars would reduce cardiovascular disease.
All trials found that lowering blood sugars with DRUGS did NOT reduce cardiovascular disease or death. This was a major problem. All of the current treatments of T2D are based on the underlying assumption that tight glucose control was beneficial. But all these trials agreed. There was no benefit.
So, why is treating blood sugars so ineffective for cardiovascular disease (atherosclerosis)?
This brings us to the LANCET trial, published in 2009 in the Journal of the American Medical Association. In this trial, researchers studied inflammatory markers hsCRP (high resolution C-Reactive Protein), IL-6 (Interleukin 6) and sTNFr2 (soluble tumor necrosis factor receptor 2). These are all markers that predict incident heart attacks and stroke. So, if lowering blood sugars was going to be beneficial, then you might expect that it would need to reduce inflammation to do so.
The point of this study was to see if insulin or metformin would reduce inflammation. This was a randomized controlled study of four groups – placebo, metformin, insulin or both with a total of 500 patients. Certainly, those drugs were able to lower blood sugars. That’s to be expected. That what they were designed for. However, does lowering blood sugars result in lower inflammation? Yeah, not so much.
Inflammatory markers were essentially unchanged despite the better sugar control. The exception is insulin treatment alone. It tends to increase hsCRP and IL-6 despite the fact that insulin is anti-inflammatory, due to the fact that, as the only glucose-lowering hormone in the body, insulin not only alleviates the detrimental effects of hyperglycemia through its metabolic regulation, but also directly modulates inflammatory mediators and acts upon immune cells to enhance immunocompetence.
But here the opposite is happening, because insulin cannot treat insulin resistance (high levels of insulin cause insulin resistance). It’s like treating alcoholic with more alcohol. Insulin makes thing worse, not better Therefore, treatment with insulin would be expected to make blood sugars (symptom) better, but make the diabetes worse.
In 2009, the NICE-SUGAR trial found that intensive glucose control increased mortality among adults in the ICU: a blood glucose target of 180 mg/dl or less resulted in lower mortality than did a target of less than 120 mg/dl. The newly published SHINE randomized trial in 2019 demonstrates that as in other conditions, targeting blood sugar less than 180 mg/dL but not tight control is the best option in patients hospitalized for strokes.
The results of a Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS) randomized 14,671 participants with type 2 diabetes and atherosclerotic cardiovascular disease (ASCVD) to sitagliptin or placebo, in addition to usual care were released in June 2015 illustrates once again the futility of targeting blood sugars in the treatment of Type 2 Diabetes. There was no cardiovascular benefit of sitagliptin.
Trials such as TECOS were designed to demonstrate cardiovascular safety of type 2 diabetes drugs in the wake of the rosiglitazone (Avandia, GlaxoSmithKline) scandal. In 2012, the U.S. Justice Department announced GlaxoSmithKline had agreed to plead guilty and pay a $3 billion fine, in part for withholding the results of two studies of the cardiovascular safety of Avandia between 2001 and 2007.
Prior to TECOS, two other dipeptidyl peptidase-4 (DPP-4) inhibitors had shown a signal for heart failure in their respective cardiovascular outcomes trials — the SAVOR study with saxagliptin (Onglyza, Bristol-Myers Squibb/AstraZeneca) and the EXAMINE trial of alogliptin (Nesina, Takeda) and both of these agents now carry warnings about heart failure on their US labels.
New research at the University of Kentucky shows that changes to mitochondria — the powerhouse of cells — drive chronic inflammation from cells exposed to certain types of fats, shattering the prevailing assumption that glucose was the culprit.
So now we can understand a little bit better the results of the ACCORD, ADVANCE, VADT, ORIGIN, TECOS and various other trials. All these trials were aimed at treating symptoms and not diseases. They treated the high blood sugar, but not the underlying insulin resistance.
Since atherosclerosis is an inflammatory disease, any treatment that may be potentially effective should somehow also reduce inflammation. Yet neither insulin nor metformin is able to lower inflammation. They can’t fight the fire, so to speak (inflammation is sometimes call ‘the fire within’). Therefore, neither insulin nor metformin was able to reduce the incidence of heart disease or stroke. Similarly, these treatments were not able to affect the underlying inflammatory cascade that is so damaging to the human body. In short – these treatments are virtually useless. It is like treating a life-threatening infection with Tylenol. Unfortunately, 99% of type 2 diabetes treatment is currently aimed at reducing blood sugars, including all the major current diabetes guidelines, even though this strategy has been proven to be useless over and over and over and over.
So, it is logical and important to lower inflammation. But, lowering blood sugars with DRUGS does not lower inflammation and cardiovascular mortality.
On the other hand, we can restore health by lowering chronic inflammation through a healthy, anti-inflammatory lifestyle by eating more fruits and vegetables, managing chronic stress and exercising regularly.
But does lowering inflammation with DRUGS will lower blood sugar or induce any health benefit?
Let’s analyze.
Over a hundred years ago, high doses of salicylates were shown to lower glucose levels in diabetic patients. The glucose-lowering effects of salicylates, seen decades ago in patients with diabetes (1–7), are now recognized as well to be due at least in part to NF-κB inhibition (8, 10, 43, 73). More recent studies demonstrated that high-dose aspirin (~7.0 g/d) improved multiple metabolic measures in patients with T2D, including substantial reductions in fasting and postprandial glucose, triglycerides, and FFAs (9). These changes were associated with reduced hepatic glucose production and improvements in insulin-stimulated glucose disposal, assessed during euglycemic-hyperinsulinemic clamping. However, the therapeutic usefulness of high-dose aspirin is limited by the antithrombotic and anti–platelet aggregation effects, which, coupled with gastrointestinal irritation, are associated with unacceptably high risks of bleeding.
Although low dose aspirin (<100 mg/d) can help prevent cardiovascular problems caused by blood clots, but it can also increase risk of bleeding. For persons with known CVD, the beneficial effect of aspirin uses for preventing cardiovascular events outweighs the harmful side effects.
Glucocorticoids display potent anti‐inflammatory effects, and are therefore frequently prescribed by physicians to treat a wide variety of diseases. But, Steroids are the main cause of drug-induced hyperglycemia. They not only exacerbate hyperglycemia in patients with known diabetes mellitus (DM), but also cause DM in patients without documented hyperglycemia before the initiation of glucocorticoids (GC) therapy, with an incidence that can reach up to 46% of patients, and increases in glucose levels up to 68% compared to baseline. Observational studies suggest that systemic absorption of topical steroids could be diabetogenic.
Ample evidence exists in support of the potent anti-inflammatory properties of statins (HMG-CoA reductase inhibitors). An important study that addressed the anti-inflammatory effect of statins was the PRINCE (pravastatin inflammation/CRP evaluation) trial, which demonstrated that oral administration of pravastatin (40mg/day) for 24 weeks significantly reduced serum CRP levels in subjects with and without CVD, independently of any changes in LDL cholesterol.
But, recent findings, which appear in the journal Diabetes Metabolism Research and Reviews, revealed that people who took statins were more than twice as likely to receive a diabetes diagnosis than those who did not take the medication. Additionally, people who took statins for longer than 2 years were more than three times as likely to develop diabetes.
So, targeting inflammation with statins does not improve glycaemia and therefore does not provide an integrated anti-inflammatory approach for diabetes and CVD.
Conclusion: Lowering blood sugars or inflammation with DRUGS for reducing cardiovascular mortality is virtually useless. They make health condition worse.
Why? Why, you may ask? Well, nobody makes any $$$ when you get better, do they?
Modern medicine is devoid of cures, only expensive management of complications. “The job of these organizations is to look for a cure, but never to find one”…spot on! When effectiveness is reported honestly, the chance of adverse side effects is often greater than the chance of getting any benefit from the drug.







CAROLINA: Linagliptin, glimepiride show similar CV safety in lower-risk type 2 diabetes
Adults with early type 2 diabetes and elevated cardiovascular risk who were assigned the DPP-IV inhibitor linagliptin were no more likely to experience a CV event during 6 years of follow-up than similar adults assigned the sulfonylurea glimepiride, according to study data presented at the European Association for the Study of Diabetes annual meeting.
Researchers determined there were no between-group differences with respect to CV events. The HR for the primary outcome was 0.98 (95% CI, 0.84-1.14). Corresponding HRs for CV mortality and non-CV mortality were 1 (95% CI, 0.81-1.24) and 0.82 (95% CI, 0.66-1.03), respectively. There was no between-group difference for HbA1c.
Researchers noted that participants in the glimepiride group experienced modest weight gain vs. participants assigned linagliptin (between-group difference, –1.5 kg; 95% CI, –1.8 to –1.3) and experienced greater incidence of investigator-reported hypoglycemia (37.7% vs. 10.6%), for an HR for hypoglycemia of 0.23 for linagliptin vs. glimepiride (95% CI, 0.21-0.26), or a number needed to treat of three over 6 years. Patients in the glimepiride group also experienced more severe hypoglycemia vs. those assigned linagliptin (2.2% vs. 0.3%).
Adverse events occurred for 2,822 participants in the linagliptin group (93.4%) and 2,856 in the glimepiride group (94.9%), with 15 participants in the linagliptin group vs. 16 in the glimepiride group experiencing confirmed acute pancreatitis.
Based on the totality of the data from CAROLINA and CARMELINA, the FDA should revisit the glimepiride product label warnings for increased CV mortality.
Good Info
I was diagnosed with Type2 Diabetes and managed to reverse it and keep control of my blood sugar levels.
some good detail here http://giftslate.com/diabetes